Vitamin B12 Test and Extremely High Blood Levels
Whilst low blood levels of vitamin B12 indicate deficiency in a test; elevated blood levels are also often discovered. Figures above 900 pg/ml are considered high, but certain cases have recorded four or even five figure values. What do these figures mean – and are such levels a cause for concern?
High B12 levels in the blood are not necessarily a reason to panic, as they can stem from a number of different causes. They should however be investigated, as some of the possible underlying causes include severe diseases. Alongside alcoholism, genetics, malabsorption and increased transport molecules in the blood; diseases of the liver, kidneys and the blood (such as leukaemia) can be considered potential reasons for an increased B12 blood level (1-4).
Causes of High Vitamin B12 Blood Levels
Increased levels of vitamin B12 can exist for a number of reasons, which can be divided roughly into the following categories:
- Distorted results
- Testing too soon after taking B12 supplements
- The body’s failure to utilise B12 (5)
- Severe diseases (4, 5)
This article will take a closer look at the causes of elevated B12 blood levels, as well as considering the necessary ways to respond. At the end, there is also a guide of what to do if this is the case.
Distorted Results
It is now known that the test results of numerous laboratories are distorted if the patient has a very high number of intrinsic factor (IF) antibodies in the blood. The test then shows extremely high values beyond 1000 pg/ml of B12, although in reality there could well be an extreme vitamin B12 deficiency present (27-29).
A check for IF antibodies, homocysteine and MMA in the urine can thus indicate whether the high values of B12 have been mistakenly produced.
The Importance of Time Intervals
A very common reason for high B12 levels is because the blood test has been carried out too soon after the administration of a B12 injection. This should be avoided and tests should be delayed by 7-10 days post-injection. Results can otherwise be very misleading, as B12 that has not yet been metabolised elevates the blood level. Nonetheless, high B12 levels are absolutely harmless in these cases.
Taking high-dose oral B12 supplements can also greatly increase blood levels – here, the same period of 7-10 days should be observed before testing.
Should high blood levels occur during a course of vitamin B12, then another measurement should be taken 10 days after supplementation has ended.
Usage Problems: Vitamin B12 Deficiency Despite High Blood Levels
If B12 values remain extremely high in a second blood test, the cause can often be difficult to determine, however, is likely related to utilisation problems within the body.
These problems occur when the body is not capable of properly utilising vitamin B12, leaving it to accumulate in the blood. It is therefore possible to be B12 deficient despite having high B12 blood levels – for example, if the vitamin cannot correctly bind to transport molecules (6). This can be tested using a holo TC or MMA urine test, which only measure the usable B12 (holo TC) or the metabolic product (MMA test).
Checking the Vitamin B12 Status with an MMA Urine Test
High vitamin B12 blood levels which have not been caused by a mistimed test should always be followed up by an official B12 status check. The most comfortable way of doing this is by measuring the methylmalonic acid (MMA) in the urine, which determines how much vitamin B12 the cells actually receive. The test can be carried out comfortably and quickly at home; though must be ordered online and can be expensive.
High Blood Levels and Vitamin B12 Transport Molecules
Another method that requires a visit to the doctor for a blood test is the holo TC test, which only measures vitamin B12 that is bound to the transport molecules, transcobalamin. Only this bound form of B12 can be correctly transported to the tissue and body store and thus utilised by the body (7, 8). While free, unbound B12 can produce high levels in a serum test; it has no biological function whatsoever.
Multiple forms of the transcobalamin transport molecule exist – the one that is important here is transcobalamin II, as it allows B12 to become biologically available. The holo TC test only measures B12 that is attached to transcobalamin II, thus giving a much better indication of the available supply.
Below is a list of the most common usage problems in relations to transport molecules:
Deficiency of Transcobalamin II
Certain rare hereditary diseases lead to a deficiency of transcobalamin II, meaning that a vitamin B12 deficiency can emerge despite a good supply. Here, B12 serum levels appear very high, despite the fact that a deficiency is present.
Transcobalamin II Antibodies
Hereditary illnesses and the long-term use of B12 injections can sometimes trigger the production of antibodies that work against transcobalamin II, leading to the vitamin not being utilised properly (9).
Transcobalamin Bonding Problems
In this instance, transcobalamin is fully available but has problems bonding with vitamin B12 – there will thus also be a B12 deficiency, despite very high blood levels.
Overproduction of Haptocorrin
Finally, some cases show the over production of other molecules which also bond to vitamin B12, most commonly the so-called haptocorrin or R-binder, to which transcobalamin I and III belong. As a result, B12 bonds to these molecules instead of transcobalamin II; while serum values of B12 seem to rise, none of the B12 is available for the body to use.
High Vitamin B12 Blood Levels and Diseases
Sometimes high blood levels can be attributed to serious diseases. The following mechanisms are responsible for high vitamin B12 blood values in such diseases:
- Overproduction of haptocorrin
- Mistaken excretion of vitamin B12
- Release of large quantities of B12 from the body’s store in the liver
- Production of B12 analogues through bacterial overgrowth
Below is a list of the most common diseases associated with very high vitamin B12 blood levels.
Disease | Mechanism |
Cancer and tumours (4) | |
Liver tumours
|
|
Other tumours (12)
|
|
Blood diseases | |
Chronic myelogenous leukaemia (CML) (14) | Elevated production of granulocytic haptocorrin |
Polycythemia vera (PV, Polycythemia, PCV) (15, 16) | Increased release of granulocytic haptocorrin |
Myelofibrosis (osteomyelofibrosis, OMF, bone marrow fibrosis) | Increased production of transcobalamins |
Hypereosinophilic syndrome (HES) (17) | Elevated production of haptocorrin |
Acute leukaemia | Increased production of haptocorrin |
Liver diseases | |
Hepatitis (18) |
|
Liver cirrhosis | Deficiency in absorption of vitamin B12 by the liver |
Alcoholic liver disease (19, 20) |
|
Kidney diseases | |
Kidney failure (21) | Deficiency in excretion of vitamin B12 and consequent accumulation in the blood |
Intestinal diseases | |
Bacterial overgrowth in the gut (22, 23) | Increased production of B12 analogues through bacteria |
High Vitamin B12 Levels due to Chronic Inflammations
High vitamin B12 blood levels are occasionally linked to autoimmune diseases that cause chronic inflammations. The mechanism here is difficult to determine, however presumably stems from an increased production of transcobalamin II (22-24). Even so, the frequency and significance of these observations are presently unclear.
Here, increased vitamin B12 levels seem to occur much less frequently than in the previously mentioned diseases; this relationship seems to play a relatively minor role, as far as current research shows.
High Vitamin B12 Blood Levels – What to do?
High B12 blood levels should always be examined further, in order to rule out any serious diseases. Often when they appear, it is due to a simple failure in measurement; normally the time period between supplementation and the blood test is too short, distorting results – certainly no cause for panic.
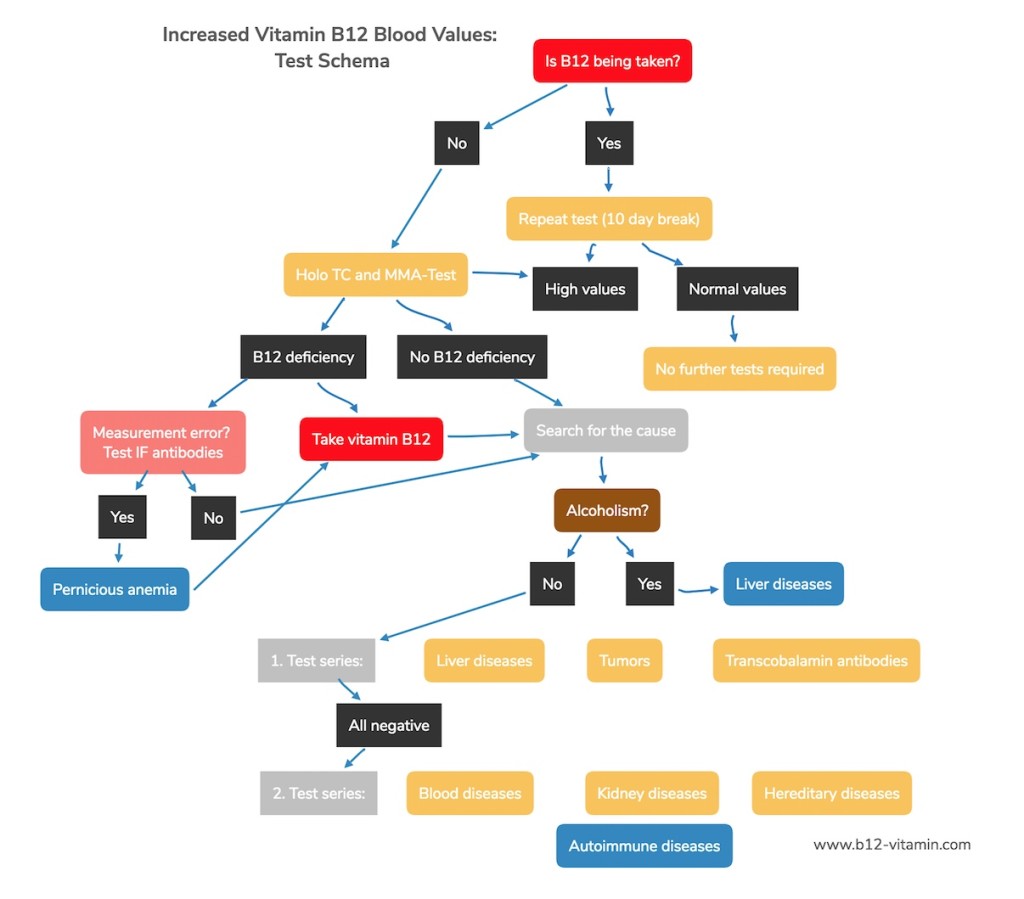
Even experienced doctors are sometimes stumped when interpreting high B12 blood values, so here is a little guide on how to proceed in such cases:
Guide to High Vitamin B12 Blood Levels
Sources
- E. Andrès, K. Serraj, J. Zhu, A.J.M. Vermorken. The pathophysiology of elevated vitamin B12 in clinical practice QJM Feb 2013
- Chiche L, Jean R, Romain F, Roux F, Thomas G, Canavese S, et al. Implications cliniques de la découverte d’une hypervitaminémie B12 en médecine interne. Rev Med Interne 2008;29:187-94.
- Arendt JFB, Nexo E . Cobalamin related parameters and disease patterns in patients with increased serum cobalamin levels. PLoS ONE 2012;9:e45979.
- Deneuville T, Mario N, Tiev KP, Tolédano C, Josselin-Mahr L, Gain M, et al. Concentration plasmatique élevée de la vitamine B12: un indicateur des maladies hépatiques ou tumourales? Rev Med Interne 2009;30 Suppl. 2:S73.
- Ermens AA, Vlasveld LT, Lindemans J. Significance of elevated cobalamin (vitamin B12) levels in blood. Clin Biochem 2003;36:585-90.
- Solomon LR. Disorders of cobalamin (vitamin B12) metabolism: emerging concepts in pathophysiology, diagnosis and treatment. Blood Rev 2007;21:113-30.
- Grasbeck R. Biochemistry and clinical chemistry of vitamin B12 transport and the related diseases. J Clin Biochem 1984;17:99-107.
- Bhatt HR, James VHT, Besser GM, Bottazzo GF, Keen H Nicolas JP, Gueant JL, Frémont S. Cobalamin binding glycoproteins. In: Bhatt HR, James VHT, Besser GM, Bottazzo GF, Keen H, editors. Advances in Thomas Addison’s Diseases. Bristol: Journal of Endocrinology Ltd; 1994. p. 253-67.
- Carmel R, Tatsis B, Baril L. Circulating antibody to transcobalamin II causing retention of vitamin B12 in the blood. Blood 1977;49:987-1000.
- Fremont S, Chamigneulle B, Gerard P, Felden P, Lambert D, Gueant JL, et al . Blood transcobalamin levels in malignant hepatoma. tumour Biol 1991;12:353-9.
- Kane SP, Murray-Lyon IM, Paradinas FJ, Johnson PJ, Williams R, Orr HA, et al. Vitamin B12 binding protein as a tumour marker for hepatocellular carcinoma. Gut 1978;19:1105-9.
- Carmel R. Extreme elevation of serum transcobalamin I in patients with metastatic cancer. N Engl J Med 1975;292:282-4.
- Gimsing P, Hippe E. Increased concentration of transcobalamin I in a patient with metastatic carcinoma of the breast. Scand J Haematol 1978;21:243-9.
- Gimsing P . Cobalamin metabolism in chronic myelogenous leukemia. Dan Med Bull 1998;45:459-79.
- Gimsing P. The cobalamin forms and analogues in plasma and myeloid cells during the course of chronic myelogenous leukemia related to the clinical condition. Br J Haematol 1995;89:812-9.
- Rachmilewitz B, Manny N, Rachmilewitz M . The transcobalamins in polycythemia vera. Scand J Haematol 1977;19:453-62.
- Zittoun J, Farcet JP, Marquet J, Sultan C, Zittoun R. Cobalamin vitamin B12 (vitamin B12) and B12 binding proteins in hypereosinophilic syndromes and secondary eosinophilia. Blood 1984;63:779-83.
- Hagelskjaer L, Rasmussen K . Methylmalonic acid concentration in serum not affected in hepatic disease. Clin Chem 1992;38:493-5.
- Lambert D, Benhayoun S, Adjalla C, Gélot MM, Renkes P, Gérard P, et al . Alcoholic cirrhosis and cobalamin metabolism. Digestion 1997;58:64-71
- Baker H, Leevy CB, DeAngelis B, Frank O, Baker ER . Cobalamin and holotranscobalamin changes in plasma and liver tissue in alcoholics with liver disease. J Am Coll Nutr 1998;17:235-8.
- Hofer LJ, Elian KM . Parenteral vitamin B12 therapy of hyperhomocysteinemia in end-stage renal disease. Med Clin Exp 2004;27:10-3.
- Murphy, M. F., Sourial, N. A., Burman, J. F., Doyle, D. V., Tabaqchali, S. and Mollin, D. L. (1986), Megaloblastic anaemia due to vitamin B12 deficiency caused by small intestinal bacterial overgrowth: possible role of vitamin B12 analogues. British Journal of Haematology, 62: 7–12.
- Brandt LJ, Bernstein LH, Abdul W. Production of Vitamin B12 Analogues in Patients with Small-Bowel Bacterial Overgrowth. Ann Intern Med. 1977;87:546-551.
- Molad Y, Rachmilewitz B, Sidi Y, Pinkhas J, Weinberger A . Serum transcobalamin and transcobalamin levels in systemic lupus erythematosus. Am J Med 1989;88:141-4
- Grindulis KA, Calverley M, Cox C . Rheumatoid arthritis: is serum vitamin B12 high in active disease? J Rheumatol 1984;11:211-2. MedlineWeb of Science
- Kalyoncu U, Buyukasik Y, Akdogan A, Karadag O, Bilgen SA, Kiraz S, et al. Increased serum vitamin B12 levels are associated with adult-onset Still’s disease with reactive macrophage activation syndrome. Joint Bone Spine 2010;77:131-4.